Why Your Gift Matters
Patients Found Better Lives with Answers from National Jewish Health
Patients come to National Jewish Health from around the world to receive treatment they can't find anywhere else, and we are grateful to the many patients who have shared their inspiring stories. It is our hope that their messages provide you strength and encouragement.
Transcript
Speaker 1: What shot did you get today?
Speaker 2: I got one that'll save my life.
Narrator: It has been a long, hard year. But hope is growing. Every day, people are being vaccinated against COVID-19 at National Jewish Health and across the country. This Corona virus has infected millions. Its victims have overwhelmed hospitals and communities, and this pandemic has sent shockwaves through the economy. National Jewish Health has responded, adapted, innovated, invested. Rising to the challenge of COVID-19, we have worked nonstop. We've developed and performed multiple molecular and antibody tests for five states.
Speaker 3: I saw COVID-19 patients in our acute respiratory clinic. Cared every night for acutely ill patients in 800 intensive care beds that we manage in Colorado and five Western states. We sent critical care physicians when New York's Mount Sinai hospitals and USC Keck Hospital in Los Angeles needed help. We've conducted research to clarify our understanding of SARS COVI-2 and how best to treat COVID-19.
William Janssen: Since the start of the pandemic, we have participated in over nine clinical trials. And so we're exploring a therapeutic now that can actually prevent or target the scarring in the lungs. We've made significant progress
in treating COVID. And I think it's primarily through the clinical trials that we've done that.
Speaker 3: In the laboratory, our scientists are studying just how the immune system recognizes the virus and how it's able to defeat the virus, and why sometimes its response is so fierce that it makes the patient worse. While all the while we're keeping a close eye on the viral variants that are emerging here, and around the world.
Philippa Marrack: So you have this race between the vaccines and the virus. The virus is busy mutating to try and avoid the vaccines. Well, this is Darwinian evolution, right in front of your eyes. I think the vaccines so far will cope pretty well with the variants that have shown up so far.
Reeti Khare: Right at the start of the COVID-19 pandemic, we launched antibody and PCR based testing for SARS COV-2. We're developing a PCR based assay that can monitor these variants inexpensively as they spread through the community.
Speaker 3: Even after patients had fought off the infection, debilitating symptoms can linger for months, perhaps even longer.
Raphael Sung: There are millions of people getting infected with COVID-19 United States, and we expect millions to have consequences of that infection long-term.
Speaker 3: Twenty-nine-year-old, Sarah Hutcherson suffered a relatively mild case of COVID-19. Seven months later, the former college athlete considers it an accomplishment to walk to the mailbox.
Sarah Hutcherson: My husband has to do everything. So he like makes dinner. He's doing the chores. And I just can't do that. I work for a couple hours at most, then I have to take a nap. But I'm frustrated because I'm 29, and I can't work a full day.
Speaker 3: Often at night, for no apparent reason, her heart starts racing.
Sarah Hutcherson: It's unsettling because you're like, "What's happening? I'm just lying here." There shouldn't be anything. It just comes out of the blue.
Speaker 3: Ramiro Estrada was working at a nursing home when he contracted COVID-19 so severely, that he required mechanical ventilation and an induced coma.
Ramiro Estrada: This virus, it changed my life. I don't work for nine months. I feel very happy with this hospital, because they understand what my situation was. I'm going in a good way, because I'm more strong right now.
Speaker 3: In March 2020, Tara Anne was one of the first people in Los Angeles to be diagnosed with COVID-19. Almost a year later, she still suffered debilitating symptoms.
Tara Anne: I came out here to Colorado to get treatment at National Jewish. I'm still dealing with long-term effects of it. My brain still isn't the same as it was before. My body still isn't the same as it was before. I can't breathe right. Can't think right. But prior to this, I have a very demanding job. I arranged like a lot of logistics. I traveled 250 days a year around the country and coordinated that for hundreds of people. And now I cannot draw a cube.
Raphael Sung: I have our multi-disciplinary program. It's called the Center for Post-COVID Care and Recovery, where we have neurologists, cardiologists, pulmonologists, allergists, immunologists, all working together to really try to figure out what's causing these issues, what's going to speed recovery the most, and what's going to help improve patient's quality of life.
Speaker 11: All right. You remember? You did this before, right?
Devin Shable: Yeah, our whole family tested positive for COVID in November. By mid-December, I'd say we started to experience some sort of long-hauler affects from COVID.
Janelle Shable: He has that cough that has developed, it seems, since COVID, and it's impacting him for sure. This program has been seriously phenomenal.
Devin Shable: They've been able to take a complex set of information and really drill down and look at it from every angle and try to make some conclusions.
Janelle Shable: What we've gone through in two days would have taken us probably 15 different appointments somewhere else, spread out over like three months. And to have it all put into two days has just been wonderful.
William Janssen: It was tough, but everybody pulled together. We were stretched to the breaking point, but we didn't snap.
Speaker 14: I've been waiting on this vaccine for quite some time, and I'm just here to just, to get my part, and to do my part.
Speaker 15: I literally am thrilled.
Speaker 16: I doubt I'd still be here today, if I hadn't come up here, and thank you National Jewish Health.
Speaker 3:
All of us at National Jewish Health are enormously proud to be a part of the solution to this devastating disease.
Part of what makes National Jewish Health different is the people, foundations and corporations who support the hospital’s mission. Our donors make it possible for us to help people worldwide through care and research.
Morgridge Academy
for Chronically Ill Children
Morgridge Academy is a free day school for children in kindergarten through eighth grades who are living with chronic medical conditions. It is the only school of its kind on a medical campus in the country and serves up to 90 students each school year.
 Learn more about Morgridge Academy
Learn more about Morgridge Academy
Transcript coming
Thorough and Expert Care,
Family Twice Blessed
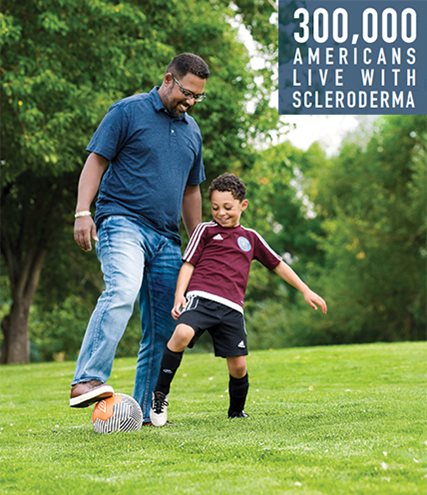
Successful treatment of David Espinosa's scleroderma inspired a return to National Jewish Health when 8-year-old Remy developed frightening episodes of breathlessness.
Your gift today will support children and adults with lung, heart, immune and related conditions.