Having COVID-19 on top of immunodeficiency requires extra special care
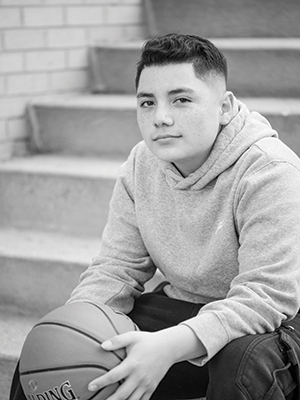 Twelve-year-old AJ Salgado-Rael has been accustomed to taking health precautions for as long as he can remember. “He was three when doctors discovered he has XLA immunodeficiency,” Sabrina Salgado-Rael, AJ’s mom, said. XLA immunodeficiency is an inherited inability to make antibodies that help fight infections. AJ receives antibody infusions regularly at National Jewish Health to strengthen his immunity.
Twelve-year-old AJ Salgado-Rael has been accustomed to taking health precautions for as long as he can remember. “He was three when doctors discovered he has XLA immunodeficiency,” Sabrina Salgado-Rael, AJ’s mom, said. XLA immunodeficiency is an inherited inability to make antibodies that help fight infections. AJ receives antibody infusions regularly at National Jewish Health to strengthen his immunity.
For AJ, COVID-19 presented a new threat to his compromised health. For this reason, the family took as many precautions as possible. However, in early June, the Salgado-Rael family felt confident about protecting AJ and took a road trip to Arizona. “We hadn’t been out of the house in three or four months,” said AJ’s mother, Sabrina. The trip went well, but on the way back, AJ began getting sick. “He was nauseous and coughing. The morning after we got home, he woke up with a fever.”
Sabrina brought AJ to National Jewish Health, where he could be tested for COVID-19 infection and get results in 24 hours. “We were very worried about AJ and wanted to know as soon as possible if he had COVID-19,” said Sabrina. “National Jewish Health was the only place we could get results so quickly.”
AJ tested positive for COVID-19. He had a strong cough and headache, slept 20 hours a day and had no appetite. AJ couldn’t receive his regular IVIG infusion, seriously threatening his immunity. Three weeks into his COVID-19 battle, however, he was able to receive his infusion at National Jewish Health in a specially equipped negative-pressure room that kept him and others safe.
Even with the infusion, AJ had trouble clearing the infection and received care in the Pediatric Acute Respiratory Clinic. Just as doctors at National Jewish Health were preparing to give AJ convalescent plasma, he finally cleared the virus. He still suffers from lingering COVID-19 symptoms, including fatigue, headaches, compromised cognitive function and nausea. His care is being managed in the Pediatric COVID Recovery Clinic at National Jewish Health.
During the multidisciplinary evaluation and treatment AJ received, doctors discovered a mild case of bronchiectasis, an inflammation and dilation of the airways likely caused by repeated respiratory infections.
“We were fortunate to detect the bronchiectasis while it was still mild,” said pediatric pulmonologist Jane Gross, MD. “We are treating it aggressively and believe we will be able to reverse the condition.”